ESC Congress 2019
Several researchers presented their latest studies at the annual Congress of European Society for Cardiology, the largest get-together of its kind. Elevating the Congress further this year was its conjunction with the World Congress of Cardiology, putting the spotlight on global cardiovascular health, highlighting differences in prevalence, clinical manifestations, prevention strategies, diagnostic modalities and management of cardiovascular diseases around the world, as stated on the ESC webpage.
PhD fellow Christine Rootwelt, MD, presented the study Apparent sex differences in risk of life-threatening events in arrhythmogenic cardiomyopathy are related to exercise habits, which concluded that sex differences in arrhythmic risk in arrhythmogenic cardiomyopathy (AC) were attributable to higher exercise doses in male AC-patients. This highlights the importance of exercise assessment in these patients, and challenges the current opinion of male sex as a risk factor in itself. Risk stratification based on sex may underestimate the risk of physically active female AC-patients.
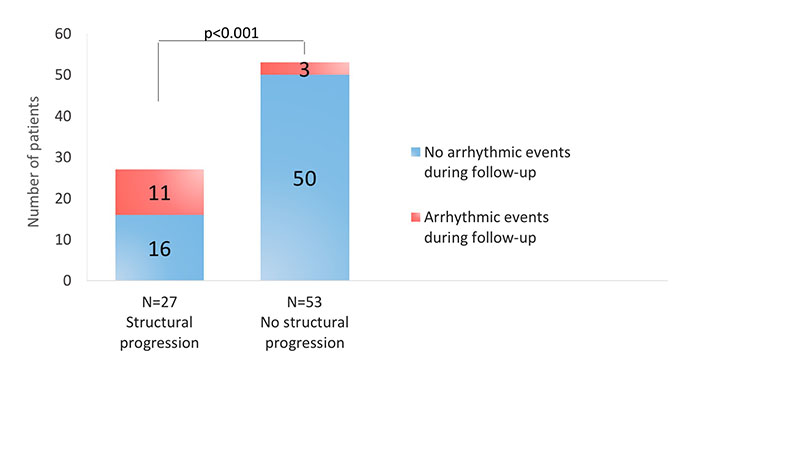
PhD fellow Monica Chivulescu, MD presented the study “Structural progression increases the risk of ventricular arrhythmias in patients with arrhythmogenic cardiomyopathy”. The study concluded that disease penetrance was fairly high in family members both at inclusion and during follow-up. Rate of progression was similar in probands and family members with arrhythmogenic cardiomyopathy and structural progression was associated with higher incidence of severe arrhythmic event in arrhythmia free patients during follow-up.
The study was simultaneously published in the European Heart Journal (https://doi.org/10.1093/eurheartj/ehz570)
Prof Perry Elliott from University College, London, United Kingdom and Benjamin Meder, University of Heidelberg, Germany talk about the study in a ESC Cardio Talk podcast available on Spotify, Apple Podcasts, Castbox, Google Podcasts, The Podcast App. (https://www.escardio.org/The-ESC/What-we-do/news/ESC-Cardio-Talk)

In a collaboration study with Akershus, Oslo and Ullevål University Hospital, Uppsala University and University of Oslo it was demonstrated that secretoneurin (SN) concentrations seem to reflect additional pathophysiology to established risk indices and improve risk assessment in patients with moderate to severe aortic stenosis (AS). First author of “Circulating secretoneurin concentrations provide incremental prognostic information to established risk indices in patients with moderate to severe aortic stenosis” was Brynildsen J. from Akershus University Hospital.
Lamin A/C dilated cardiomyopathy is a highly penetrant inheritable cardiomyopathy with some patients developing muscluar dystrophy. Studies have indicated higher morbidity and mortality in men compared to women with lamin A/C. PhD fellow Eystein Skjølsvik, MD presented the study «Sex differences in cardiac function and muscular dystrophy in lamin A/C genotype positive family members», which concluded that male lamin A/C genotype family members had earlier penetrance and more frequently impaired cardiac function compared to women. AV-block and arrhythmic disease did not differ. Muscular dystrophy was more frequent in women. These findings indicate sex differences in the phenotypical expression of lamin A/C disease.

Impact of novel echocardiographic recommendations on diastolic function in clinical practice.
Speaker: Thor Edvardsen, ESC Congress 2019, Paris, France
Professor Edvardsen stressed that the purpose of the new algorithm on diastolic function presented in the 2016 ASE/EACVI recommendations was to simplify and increase the utility in clinical practice. The other important purpose was to construct a more specific algorithm to identify elevated LV filling pressures. The latter is important and recent studies demonstrates that elevated filling pressure is present in most patients with diastolic dysfunction according to the new recommendations. The algorithm excludes reduced left ventricular ejection fraction since it is assumed to have concomitant diastolic dysfunction.
The importance of diastolic function has become evident as heart failure has become epidemical across the globe; 1 million patients are hospitalized annually in the USA alone. Approximately half of them have an ejection fraction above 50%, which has led to the need of easily available measures for LV filling pressure. Speckle tracking echocardiography has been introduced as a novel technique to improve diagnostic accuracy and estimation of filling pressures but it does need further validation in clinical studies.
Cardiac imaging for risk stratification in arrhythmias
Speaker: Kristina Haugaa, ESC Congress 2019, Paris, France
Professor Haugaa presented the interesting topic of risk stratification for first ventricular arrhythmic event and on the indications for implantable cardioverter defibrillator (ICD) implantation in primary prevention. Impaired left ventricular (LV) function reflected by reduced ejection fraction (EF) or impaired global longitudinal strain and heterogeneous LV contraction expressed by increased mechanical dispersion in those with relatively preserved EF were predictors of life threatening arrhythmic events in different cardiac conditions like ischemic heart disease, cardiomyopathies and desynchrony.
She presented several key cases where she highlighted the utility of imaging parameters in arrhythmic risk stratification.
In arrhythmogenic cardiomyopathy measurement of right ventricular (RV) free wall strain can help detection of reduced RV function beyond visual assessment and RV fractional area change. Detection of any structural abnormality in patients with AC not previously implanted with an ICD should lead to close follow up of these individuals as they carry a high arrhythmic risk.
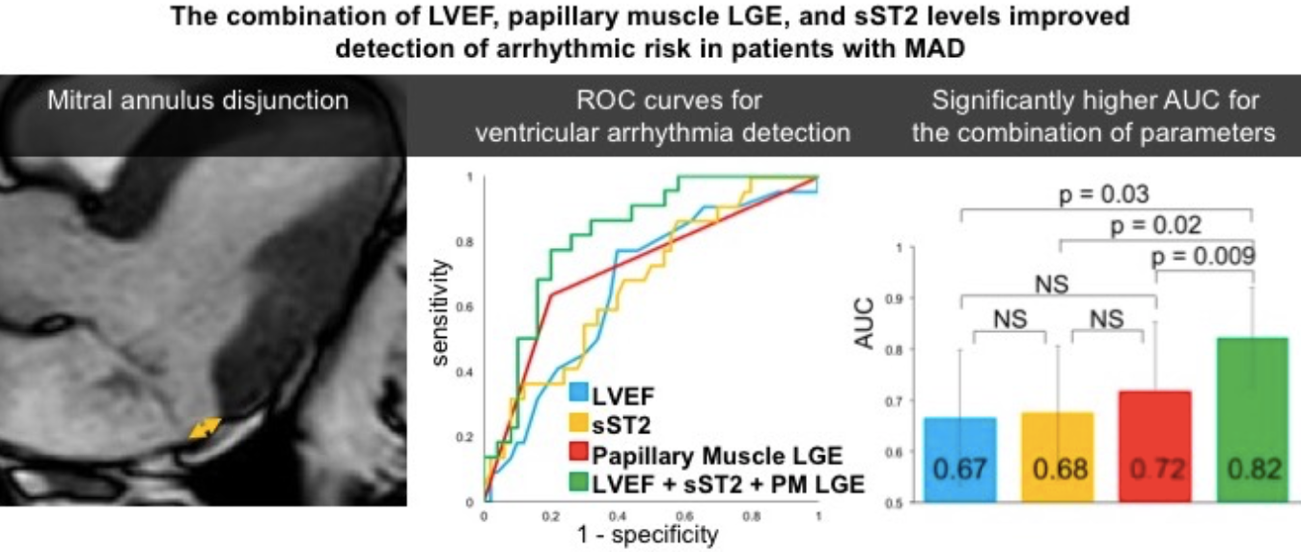
Second case was the case of a young woman with palpitation and frequent premature ventricular contractions on Holter monitoring who had mitral annulus disjunction (MAD), the gap between mitral valve and myocardium in systole. Based on previous publications, female sex, T-wave inversion and papillary muscle fibrosis and MAD are linked to increased arrhythmic risk in mitral valve prolapse and MAD itself is associated with high arrhythmic risk irrespective of mitral valve prolapse.
Abstracts presented at the ESC Congress
Authors: C Rootwelt1 , ØH Lie1 , LA Dejgaard1 , T Edvardsen1 , KH Haugaa1
1Oslo University Hospital, Department of Cardiology, Rikshospitalet, and Center for Cardiological Innovation - Oslo - Norway
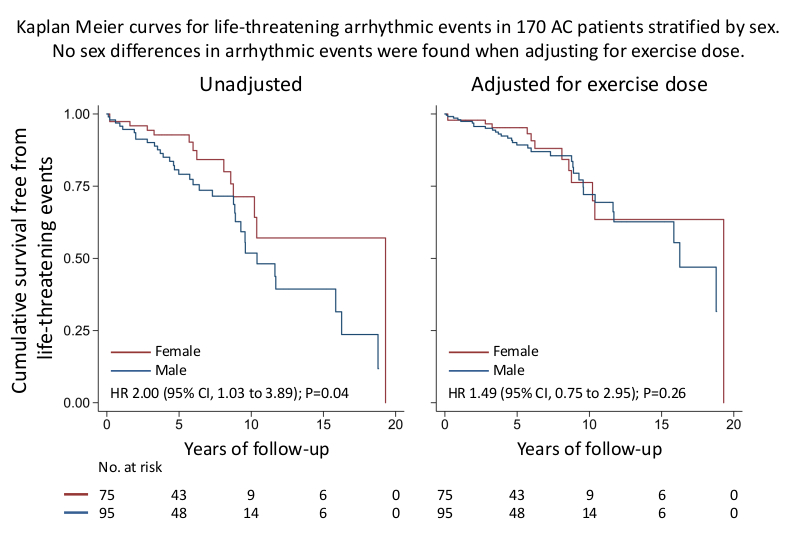
Background: Arrhythmogenic cardiomyopathy (AC) is an inheritable heart disease characterized by high risk of ventricular arrhythmias and exercise intolerance. Male sex is associated with higher risk of life-threatening events. However, this may be challenged by the fact that men exercise more than women.
Purpose: To assess whether the sex differences in arrhythmic outcome in AC-patients are driven by sex differences in exercise exposure.
Methods: We included AC-patients diagnosed between 1997 and 2017 in a longitudinal cohort study. We assessed exercise habits during the preceding 3 years before inclusion, and exercise dose was expressed as metabolic equivalent hours per week (MET-hours/week). Life-threatening events were defined as sustained ventricular tachycardia, aborted cardiac arrest or appropriate therapy from an implantable cardioverter-defibrillator at the time of diagnosis and prospectively during follow-up.
Results: We included 170 AC-patients (52% probands, 44% female, age 41±16 years). Males had higher exercise doses than female patients (36 [IQR, 14 to 54] vs. 12 [IQR, 8 to 22] MET-hours/week; P<0.001). Fifty-seven patients (34%) had previous life-threatening events, and 45 (26%) had life-threatening events during 5.7 (IQR, 2.8 to 9.4) years of follow-up. Male sex seemed to be a marker of previous life-threatening events (OR 2.0 [95% CI, 1.0 to 3.8]; P<0.05), but not when adjusted for exercise dose (Adjusted OR 1.3 [95% CI, 0.6 to 2.7]; P=0.44). Male sex also seemed to be a predictor of life-threatening events during follow-up (HR 2.0 [95% CI 1.0 to 3.9]; P=0.04) (Figure, left panel), but not when adjusted for exercise dose (Adjusted HR 1.5 [95% CI 0.8 to 3.0]; P=0.26) (Figure, right panel).
Conclusions: Sex differences in arrhythmic risk in AC were attributable to higher exercise doses in male AC-patients. This highlights the importance of exercise assessment in these patients, and challenges the current opinion of male sex as a risk factor in itself. Risk stratification based on sex may underestimate the risk of physically active female AC-patients.
Authors: J Brynildsen1 , PL Myhre1 , MN Lyngbakken1 , LG Klaeboe2 , M Stridsberg3 , G Christensen4 , T Edvardsen2 , T Omland1 , H Rosjo1
1University of Oslo, Akershus University Hospital, Department of Medicine - Lorenskog - Norway , 2University of Oslo, Oslo University Hospital, Department of Cardiology, Rikshospitalet - Oslo - Norway , 3Uppsala University, Department of Medical Sciences - Uppsala - Sweden , 4University of Oslo, Institute for Experimental Medical Research, Ulleval University Hospital - Oslo - Norway ,
Background: Secretoneurin (SN) concentrations provide important prognostic information in patients with myocardial dysfunction. Whether preoperative SN concentrations improve risk assessment in patients with moderate to severe aortic stenosis (AS) is unknown.
Methods: We included 57 patients with moderate to severe AS referred for presurgical evaluation and recorded all-cause mortality during follow-up. All patients were examined with comprehensive echocardiography, electrocardiogram (ECG), and high-sensitivity cardiac troponin T (hs-TnT) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) measurements.
Results: Median (quartile 1-3) SN concentration in the AS patients was 141 (121-163) pmol/L. Lower estimated creatinine clearance and use of diuretics, but not standard ECG or echocardiographic indices and cardiac biomarkers, were associated with increasing SN concentrations. In total, 15 patients (26%) died during 3.5 years median follow-up. SN concentrations were higher in non-survivors than survivors: 156 (133-209) vs. 140 (116-155) pmol/L, p=0.007. The optimal cut-off concentration for SN in discriminating long-term mortality was 147 pmol/L (sensitivity 67% [95% CI 38-88%], specificity 74% [58-86%]) and patients with SN concentrations above the optimal cut-off had worse prognosis than patients below the cut-off (Figure; p=0.005 with the log-rank test). Higher SN concentrations were associated with increased risk of mortality after adjustment for clinical risk factors, echocardiographic and ECG variables, hs-TnT and NT-proBNP concentrations, and whether patients were subjected to aortic valvular surgery (n=34): hazard ratio per lnSN 15.13 (95% CI 1.05-219.00); p=0.046. Receiver operating characteristics area under the curve for SN to predict mortality was 0.74 (95% CI 0.60-0.88) compared to 0.73 (0.59-0.87) for hs-TnT and 0.67 (0.51-0.82) for NT-proBNP.
Conclusions: SN concentrations seem to reflect additional pathophysiology to established risk indices and improve risk assessment in patients with moderate to severe AS.
Authors: E Skjolsvik1 , LAD Dejgaard1 , ØH Lie1 , LG Klaboe1 , NE Hasselberg1 , K Orstavik2 , T Edvardsen1 , KH Haugaa1
1Oslo University Hospital, Department of cardiology and Center for Cardiological Innovation - Oslo - Norway, 2Oslo university hospital Rikshospitalet, Department of neurology - Oslo - Norway
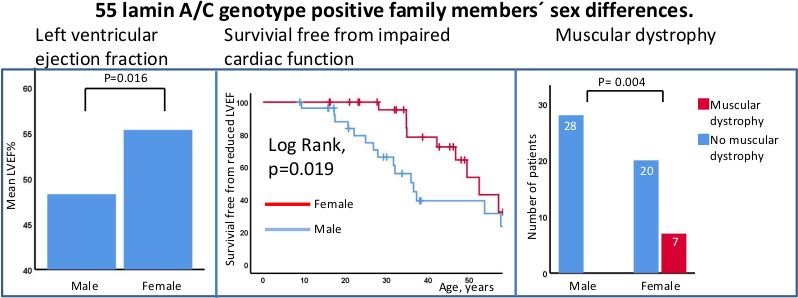
Background: Lamin A/C dilated cardiomyopathy is a highly penetrant inheritable cardiomyopathy with some patients developing muscluar dystrophy. Studies have indicated higher morbidity and mortality in men compared to women with lamin A/C.
Purpose: To explore sex differences in cardiac function, arrhythmias and muscular dystrophy in lamin A/C genotype positive family members of lamin A/C probands.
Methods: We included consecutive lamin A/C genotype positive family members recruited for cardiological evalutation based on the identification of lamin A/C genotype by cascade genetic screening. Cardiac function was assessed by echocardiography. Impaired cardiac function was defined according to guidelines as left ventricular ejection fraction (LVEF) < 52% in men, <54% in women. Presence of AV-block, atrial fibrillation and ventricular arrhythmias were evaluated by12-lead ECG, Holter monitoring, and interrogation of cardiac implantable electronic devices. Presence of muscular dystrophy was assessed retrospectively from medical records, and defined as present or not based on description of typical symptoms and/or findings on neurological exam.
Results: We included 55 lamin A/C genotype positive family members (age 35±15 years, 49% female). Men were younger at time of evaluation (31±15years vs. 40±14 years, p=0.047). Despite lower age, men had significantly lower LVEF (48±12% vs. 55±9%, p=0.016) (Figure left panel), and showed worse survival free from impaired cardiac function compared to women (log rank p=0.019) (Figure, mid panel). Male sex was a marker for impaired cardiac function when adjusted for age (adjusted OR 5.3[95%CI;1.5-18.8]) . Women had higher prevalence of muscular dystrophy compared to men (35% vs. 0%, p=0.004) (Figure right panel). We observed no sex related differences for AV-block, atrial fibrillation, nor ventricular arrhythmias.
Conclusions: Male lamin A/C genotype family members had earlier penetrance and more frequently impaired cardiac function compared to women. AV-block and arrhythmic disease did not differ. Muscular dystrophy was more frequent in women. These findings indicate sex differences in the phenotypical expression of lamin A/C disease.
Authors: M Chivulescu1 , ØH Lie1 , H Skulstad1 , BA Popescu2 , RO Jurcut2 , T Edvardsen1 , K Haugaa1
1Oslo University Hospital - Oslo - Norway ,2Institute of Cardiovascular Diseases Prof. C.C. Iliescu - Bucharest - Romania
Background: Arrhythmogenic cardiomyopathy (AC) is an inheritable cardiomyopathy with incomplete penetrance, variable phenotype severity and poorly described disease progression. It is characterized by high risk of life-threatening ventricular arrhythmias and sudden cardiac death in young individuals. Risk stratification and selection of patients presenting without history of life-threatening arrhythmic events for cardioverter-defibrillator implantation in primary prevention remains challenging.
Purpose: We aimed to assess the impact of disease progression on arrhythmic outcomes in AC patients.
Methods: We included consecutive AC probands and mutation-positive family members with at least one complete follow-up evaluation. Echocardiographic and electrical parameters were defined according to the 2010 Revised Task Force criteria at inclusion and at last follow-up. Structural progression was defined as development of new echocardiographic diagnostic criteria. Electrical progression was defined as the development of new diagnostic depolarization, repolarization and/or premature ventricular complex count criteria during follow-up. Non-sustained ventricular tachycardia or ventricular tachycardia occurring during follow-up defined incident ventricular arrhythmic events.
Results: We included a total of 144 patients (48% female, 47% probands, 40±16 years old). At inclusion, 54 patients (37%) had a history of arrhythmic events, 30 patients (21%) had overt structural disease and 114 (79%) had no or minor structural disease. During 7.0 (IQR: 4.5 to 9.4) years of follow-up, 49 patients (43%) with no or minor structural disease at inclusion developed new structural criteria being defined as progressors. Among 80 participants with no or minor structural disease and no arrhythmic history at inclusion, a first arrhythmic event occurred in 14 (17%). The incidence of arrhythmic events was higher in progressors (11/27, 41%) than in non-progressors (3/53, 6%) (p<0.001) (Figure). Structural progression was associated with higher risk of first arrhythmic events during follow-up when adjusted for sex, age at inclusion and follow-up duration, independent of electrical progression (7.6, 95% CI [1.5, 37.2], P=0.01).
Conclusion: Almost half of patients without overt structural cardiac disease at genetic diagnosis develop new structural criteria during 7 years follow-up and 17% experienced their first ventricular arrhythmic event. Structural progression was independently associated with ventricular arrhythmic events during follow-up. These findings highlight the increased risk of arrhythmias when structural abnormalities are detected. Their finding may initiate the evaluation for primary prevention cardioverter-defibrillator implantation.
Increased levels of sST2 in patients with mitral annulus disjunction and ventricular arrhythmias
Authors: E Scheirlynck1, L Dejgaard2, E Skjolsvik2, OH Lie2 A Motoc1, E Hopp3, K Tanaka4, T Ueland5, M Ribe2, C Collet1, T Edvardsen2, S Droogmans1, B Cosyns1, K Haugaa2
1University Hospital (UZ) Brussels, Centrum voor Hart en Vaatziekten Brussels Belgium, 2Center for Cardiological Innovation Oslo Norway, 3Oslo University Hospital, Radiology and nuclear medicine Oslo Norway, 4University Hospital (UZ) Brussels, Radiology Brussels Belgium, 5Oslo University Hospital, Research institute of internal medicine Oslo Norway
Background: Mitral annulus disjunction (MAD), a basal displacement of the mitral valve annulus, is described as a possible aetiology of sudden cardiac death. Stretchinduced fibrosis in the subvalvular apparatus has been suggested as the substrate of arrhythmias.
Purpose: We hypothesized that the stretch related biomarker soluble Suppression of Tumorigenicity2 (sST2) is a marker of ventricular arrhythmias in patients with MAD.
Methods: We included patients with =1 mm MAD on cardiac magnetic resonance imaging, and recorded left ventricular ejection fraction (LVEF) and late gadolinium enhancement (LGE) suggesting papillary muscle fibrosis. Circulating levels of sST2 were assessed by blood sampling. The occurrence of ventricular arrhythmias, defined as aborted cardiac arrest, sustained or nonsustained ventricular tachycardia, was assessed retrospectively.
Results: We included 72 patients with MAD [55 (3562) years old, 48 (67%) female], of which 22 (31%) had ventricular arrhythmias. Patients with ventricular arrhythmias had lower LVEF (60 ± 6 % vs. 63 ± 6 %, p=0.04), more prevalent papillary muscle fibrosis [14 (64%) vs. 10 (20%), p < 0.001] and higher sST2 levels [31.6 ± 10.1 ng/mL vs. 25.3 ± 9.2 ng/mL, p=0.01] compared to those without. Combining sST2level, LVEF and papillary muscle fibrosis optimally detected individuals with arrhythmias (area under the curve 0.82, 95%CI 0.730.92) and improved the risk model (p < 0.05) compared to individual parameters (Figure right panel).
Conclusion: Circulating sST2 levels were higher in patients with MAD and ventricular arrhythmias compared to patients without arrhythmias. Combining sST2, LVEF and LGE may improve risk stratification in patients with MAD.
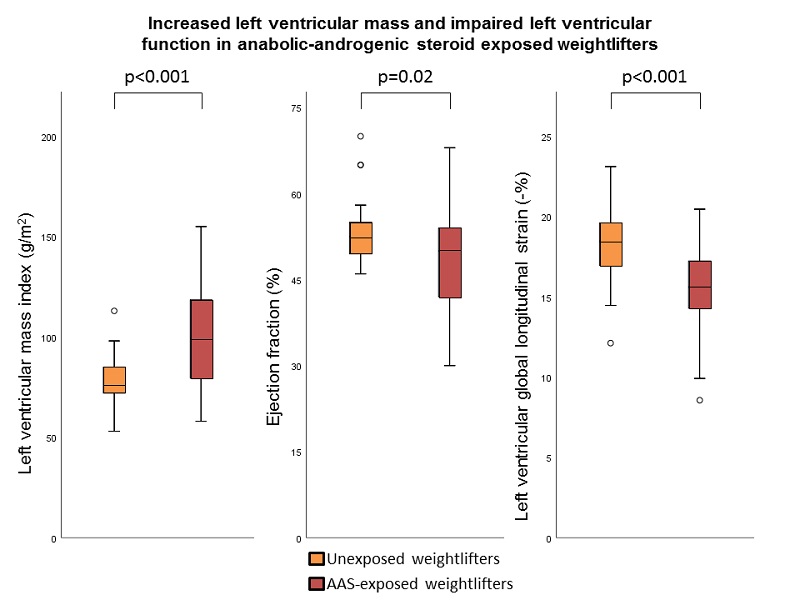
Long-term use of anabolic-androgenic steroids in male weightlifters is associated with left ventricular systolic dysfunction
Authors: R Abdullah1 , A Bjornebekk2 , L Dejgaard3 , L Hauger2 , T Edvardsen3 , K Haugaa3 , V Almaas3
1University of Oslo - Oslo - Norway , 2Oslo University Hospital, Division of Mental Health and Addiction, National Advisory Unit on Substance Use Disorder Treatment - Oslo - Norway , 3Oslo University Hospital, Department of Cardiology, Rikshospitalet - Oslo - Norway
Background: Illicit use of anabolic-androgenic steroids (AAS) is widespread and has adverse psychological and cardiovascular effects. Few well-powered studies have explored the effect of long-term AAS-use on left ventricular systolic function.
Purpose: To explore the relationship between long-term use of AAS and left ventricular mass and systolic function.
Methods: We included male weightlifters with a history of >1 year of cumulative AAS-use and male weightlifters unexposed to AAS. We performed echocardiography in all and assessed left ventricular mass using 2D echocardiographic linear measurements and Cube formula, left ventricular ejection fraction (EF) ad modum Simpson, and left ventricular global longitudinal strain (GLS) by speckle-tracking echocardiography.
Results: We recruited 100 male weightlifters, 58 of whom were previous or current AAS-users with mean±SD AAS-use of 10.4±7.0 years, and 42 unexposed weightlifters. There were no difference in age (35.5±9.2 vs. 35.3±7.5 years, p=0.8) nor body mass index (BMI) (BMI 31.4±5.0 vs.30.1±3.5, p=0.6) between AAS-exposed and unexposed weightlifters. Compared with unexposed weightlifters, AAS-exposed weightlifters demonstrated thicker interventricular septum (11.2±2.4 vs. 9.2±1.3 mm, p<0.001), thicker left ventricular posterior wall dimension (10.1±2.1 vs. 8.9±1.3 mm, p<0.001), and higher left ventricular mass index (99.7±25.4 vs. 78.4±12.1 g/m2, p<0.001). Both left ventricular EF and left ventricular GLS were decreased in AAS-exposed weightlifters compared with unexposed weightlifters (49±9 vs. 53±6%, p=0.02, and -15.6±2.6 vs. -18.3±2.1%, p<0.001) (Figure).
Conclusion: AAS use in male weightlifters was associated with increased left ventricular mass and impaired left ventricular systolic function. Our results suggest considerable adverse cardiac effects of AAS use, but the results need confirmation in prospective observational trials.
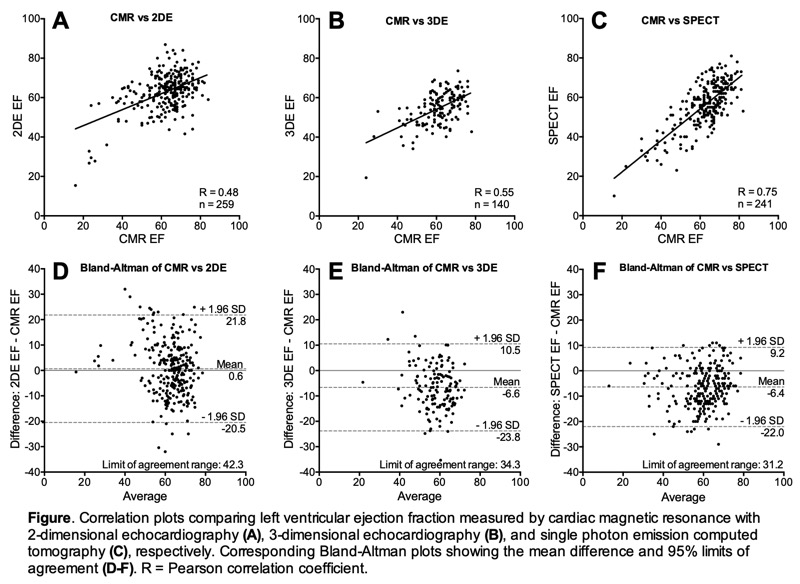
Authors: TM Stokke1 , SI Sarvari2 , AW Bjerring1 , KH Haugaa1 , MT Elahi3 , SI Hoedemakers3 , F Rademakers4 , M Monaghan5 , R Sicari6 , J Engvall7 , E Nagel8 , JL Zamorano9 , H Ukkonen10 , J D'hooge3 , T Edvardsen1
1Center for Cardiological Innovation, Department of Cardiology, Oslo University Hospital and University of Oslo - Oslo - Norway , 2Center for Cardiological Innovation, Department of Cardiology, Oslo University Hospital - Oslo - Norway , 3KU Leuven, Lab on Cardiovascular Imaging and Dynamics - Leuven - Belgium , 4University Hospitals (UZ) Leuven, Department of Cardiovascular Sciences and KU Leuven - Leuven - Belgium , 5Kings College Hospital, Department of Non-invasive Cardiology - London - United Kingdom of Great Britain & Northern Ireland , 6Institute of Clinical Physiology (IFC) - Pisa - Italy , 7Linkoping University, Department of Clinical Physiology and Department of Medical and Health Sciences - Linkoping - Sweden , 8University Hospital Frankfurt, Institute for Experimental and Translational Cardiovascular Imaging - Frankfurt am Main - Germany , 9University Hospital Ramon y Cajal de Madrid, Cardiovascular Imaging Unit - Madrid - Spain , 10Turku University Hospital, Department of Medicine - Turku - Finland ,
Background: Clinical treatment strategies are often based on measurement of left ventricular ejection fraction (LVEF). There is limited evidence about variations in LVEF when measured by different imaging modalities.
Purpose: To investigate the intermodality variability of LVEF measured by two-dimensional echocardiography (2DE), three-dimensional echocardiography (3DE), cardiac magnetic resonance (CMR), and single photon emission computed tomography (SPECT) in patients with chronic coronary artery disease (CAD).
Methods: Patients from a multicenter study (DOPPLER-CIP - Determining optimal noninvasive parameters for the prediction of left ventricular remodeling in chronic ischemic patients) with chronic CAD were included. LVEF was measured by CMR and at least one additional modality. In each modality, LVEF was measured by a core laboratory independently of the other modalities. Measurements of LVEF by CMR were compared to 2DE, 3DE and SPECT using correlation and Bland-Altman plots.
Results: A total of 343 patients were included. Mean age was 63.9 ± 8.3 years and 253 (74%) were males. Mean LVEF by CMR was 61.8 ± 11.6%. Correlations between CMR LVEF and other modalities were moderate for 2DE and 3DE, and good for SPECT (Figure A-C). CMR had significantly greater correlation to SPECT, compared to 2DE and 3DE. Bland-Altman plots indicated relatively wide limits of agreement between all modalities, ranging from 31% to 42% (Figure, D-F). Mean absolute difference of LVEF between CMR and other modalities were 8.5% for 2DE, 9.0% for 3DE, and 8.3% for SPECT. The percentage of measurements that fell within a range of 5% difference compared to CMR LVEF was 41% for 2DE, 34% for 3DE and 37% for SPECT (all p > 0.05).
Conclusions: In a multicenter study with chronic CAD patients, LVEF assessed by CMR had better correlation to SPECT, compared to 2DE and 3DE. However, there was considerable variability among all three modalities that were compared to CMR. Awareness of these variations are important in clinical management.
Authors: AW Bjerring1 , SD Fossa2 , HS Haugnes3 , KH Haugaa1 , T Edvardsen1 , SI Sarvari1
1Oslo University Hospital, Center for Cardiological Innovation - Oslo - Norway , 2The Norwegian Radium Hospital - Oslo - Norway , 3University Hospital of North Norway, Department of Oncology - Tromso - Norway
Background: Cisplatin-based chemotherapy (CBCT) is essential in the treatment of testicular cancer (TC), and platinum can be detected in TC survivors decades after cessation of treatment. CBCT has been implicated as a risk factor in cardiovascular morbidity and mortality.
Purpose: Our study aimed to assess the relationship between residual serum platinum concentrations and changes in cardiac function and morphology in TC survivors 30 years after CBCT.
Methods: Seventy TC survivors diagnosed and treated with CBCT (1980-1994) were recruited from the longitudinal Norwegian Cancer Study in Testicular Cancer Survivors. Serum platinum concentration was measured twenty years after CBCT. Patients were then allocated to either a high or low platinum concentration group. Echocardiography was performed in all subjects.
Results: The participants were on average 60±9 years old. There was a trend towards smaller left ventricular (LV) volumes in the high residual platinum concentration group (Table). No intergroup difference in cardiac function was found. Six (9%) participants had reduced EF (<52%) and 14 (20%) participants had reduced LV global longitudinal strain (> -18.0%), however, there was no intergroup difference. Neither cumulative cisplatin dose nor residual serum platinum concentration showed any correlation with LV or right ventricular functional parameters.
Conclusion: Our 30-year follow-up study of testicular cancer patients could not demonstrate impact on cardiac function caused by cumulative cisplatin dose or residual serum platinum concentrations.
|
Low residual Pt concentration |
High residual Pt concentration |
p-value |
|
|
Cumulative cisplatin dose, mg/m2 |
680±249 |
814±271 |
<0.05 |
|
Residual Pt concentration, ng/L |
44±22 |
136±44 |
<0.001 |
|
3D LV end-diastolic volume, ml/m2 |
66±17 |
60±8 |
0.07 |
|
3D LV end-systolic volume, ml/m2 |
29±15 |
24±5 |
0.08 |
|
3D ejection fraction, % |
57±9 |
59±6 |
0.24 |
|
LV global longitudinal strain, % |
- 19.2±3.3 |
- 20.0±2.0 |
0.26 |
|
LV global circumferential strain, % |
- 21.1±4.2 |
- 22.1±1.8 |
0.30 |
|
E/e’ |
10.6±4.4 |
9.2±2.2 |
0.10 |
|
TAPSE, mm |
2.2±0.4 |
2.3±0.4 |
0.22 |
|
RV fractional area change, % |
40±7 |
41±7 |
0.67 |
Data are presented as mean±SD. The P-values were derived from the Student’s t-test. LV, left ventricle; MV, mitral valve; Pt, platinum; RV, right ventricle; TAPSE, tricuspid annular plane systolic excursion